Introducing a Breakthrough in Breastfeeding Support: A Non-Nutritive Suckling Device
Parenthood is a remarkable journey filled with joy, challenges, and countless learning experiences. As parents, one of the most vital aspects is ensuring the well-being and nourishment of our newborns. The early days post-discharge are particularly crucial, with a primary focus on nurturing our babies' growth and development. That's why we're excited to introduce an ingenious solution developed by the experts at UCSD – the Non-Nutritive Suckling Device.
Breastfeeding, while natural, can often present challenges, leaving parents and caregivers seeking the right guidance and tools to ensure a seamless and successful experience. Our innovative non-nutritive suckling device aims to address this gap by providing essential insights into crucial breastfeeding skills, particularly during the critical days when establishing breastfeeding patterns is crucial.
We're honored to have Erin Walsh, a speech-language pathologist, singing voice specialist, and lactation consultant known for her clinical excellence in handling voice disorders and newborn feeding challenges, along with James Friend, a distinguished professor in the Department of Mechanical and Aerospace Engineering, and the esteemed holder of the Stanford S. and Beverly P. Penner Endowed Chair in Engineering, joining us to address our blog questions.
How does the low-cost non-nutritive suckling device work? Can you provide a brief overview of its design and functionality?
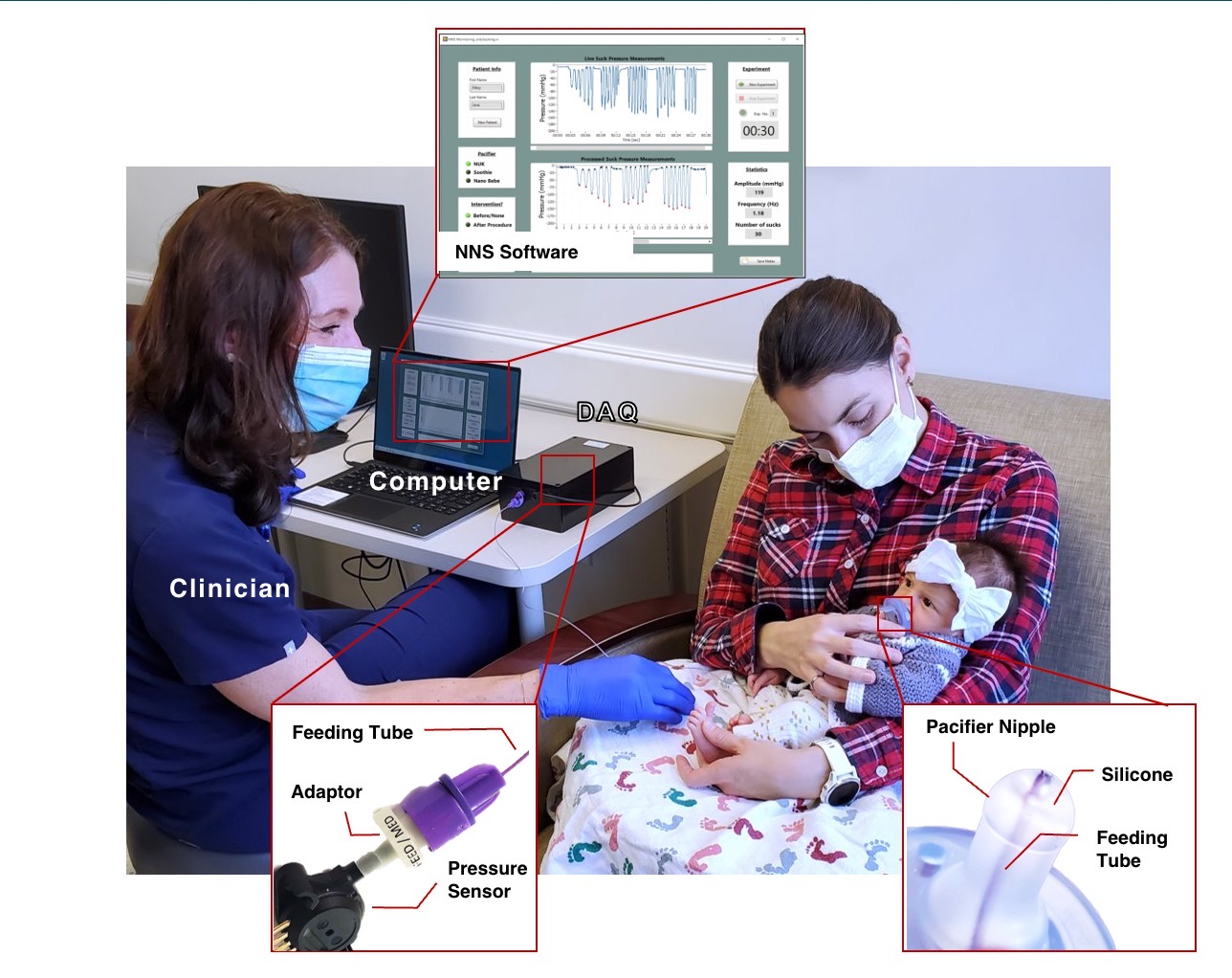
The device is an off-the-shelf pacifier that was modified with a microsensor to capture vacuum. Within 60 seconds of non-nutritive suckling we can extract features and use machine learning to identify infant suckling patterns that fall within or outside of normal ranges for healthy term newborns.
The raw data is simply a suckling vacuum measured with respect to time. The system processes this data, identifying typical features of the suckling. Babies suckle in bursts—a few suckling events then a pause—repeated for a while. The device captures the baby’s mean suckling vacuum, maximum suckling vacuum, the frequency of suckling events in a burst, the length of suckling bursts, and the overall suckling duration. After many babies’ suckling behavior has been captured, we see trends in the suckling, and discrepancies from typical suckling behavior start to appear. Machine learning helps reduce the complexity of the data, making these discrepancies extremely easy to see.
We see discrepancies in the frequency of suckling, in the strength of the suckling vacuum, the length of the bursts, absence of pauses between the bursts, and variations in the suckling events. Depending on the baby, one or more of these produce a net result from the analysis that places that baby outside the group of typical baby suckling behavior.
What are the potential applications of your device beyond identifying at-risk newborns and aiding in decision making regarding frenotomy? Are there other areas or aspects of infant feeding or oral-motor assessment where this technology could be beneficial?
Newborns leave the hospital with numerous screening measures such as hearing, temperature, labs and weight. The baby’s primary job upon discharge is to feed and thrive. A simple inexpensive instrumented pacifier can inform parents and clinicians on basic skills needed to latch and transfer milk during critical days when breastfeeding is established. The suckling performance is unnecessarily enigmatic which creates a burden when breastfeeding does not go smoothly.
Are there any plans to further refine or improve the device based on the insights gained from the initial study? What are your future goals or aspirations for this technology, both in terms of research and potential real-world impact?
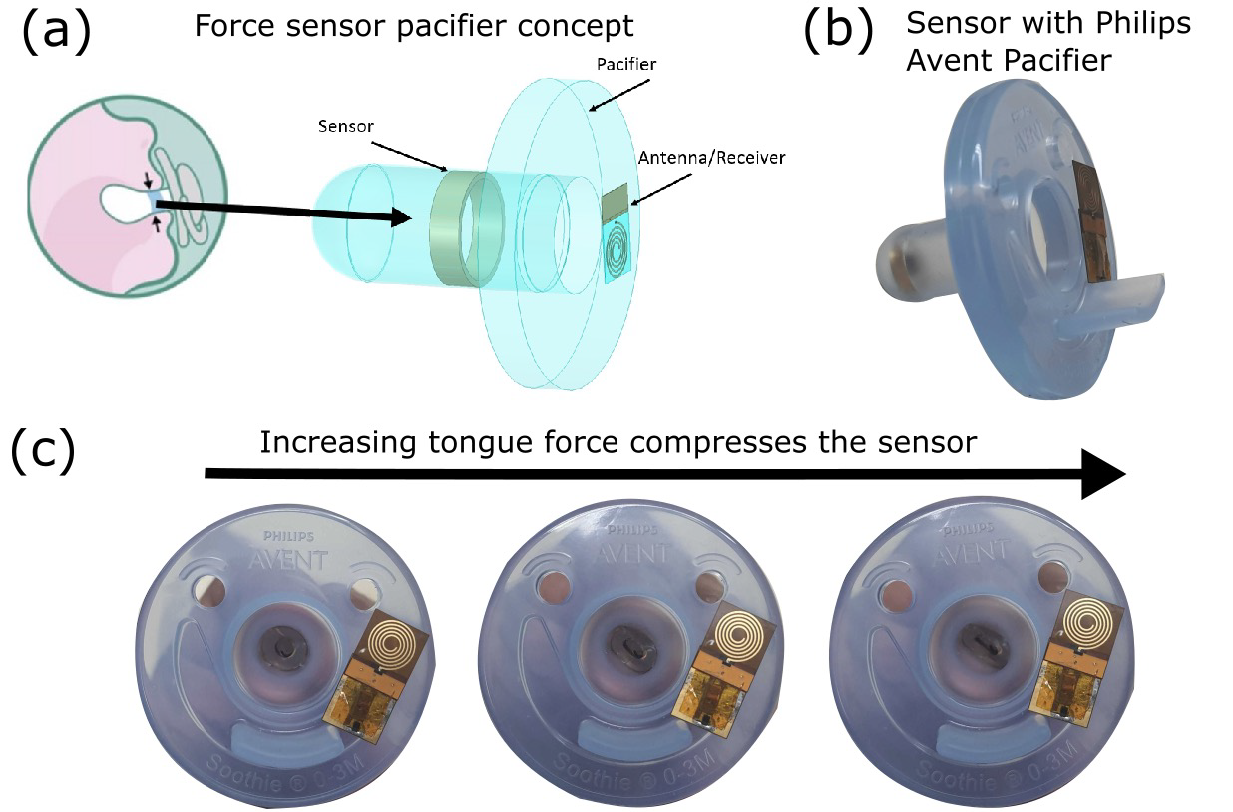
We recently added a force sensor into the pacifier that wirelessly transmits a signal into our software. This is intended to better understand ineffective milk removal and maternal discomfort associated with latching. Peering into the future, we would like to see widespread adoption of this technology as a screening tool for all infants discharged home, used for tailored therapeutic interventions by feeding clinicians, and potentially used by parents so they understand how their baby is sucking compared to age-matched peers.
Just to reference, we're thrilled to share a video featuring clinician Erin Walsh, where she provides insights into the creation of this remarkable invention. It's an excellent opportunity to gain a deeper understanding of the innovation from an expert's perspective. Feel free to watch the video to further explore the fascinating journey behind this breakthrough! Click Here to Watch the Video
And there you have it! We've uncovered the great potential of the Non-Nutritive Suckling Device, shining a light on its promising game-changing role in breastfeeding support. The synergy between experts from various domains has resulted in a solution that's all about empowerment – for parents and professionals alike.
With this groundbreaking device leading the way, we're excited to see the potential positive impact it'll make on the lives of little ones and their families.
Thanks for joining us on this post, and keep an eye out for more exciting updates in the world of healthcare and technology!
UC San Diego ACTRI